Description
Features of Epidural Needle
-
Blunt Tip Design
The tip of the epidural needle is rounded or dull rather than sharp, which helps in preventing accidental puncture of the dura mater (the membrane surrounding the spinal cord). While reducing the risk of cerebrospinal fluid leakage or CSF leakage.
-
Large Gauge Size
The Tuohy Needle is a specially designed needle with beveled & blunt tip, designed to enter in the Epidural Space. It has a large gauge size, ranging from Diameter 16G – Diameter 27G, to accommodate the passage of an epidural catheter. The standard length of tuohy needle ranges from 8 cm –10 cm for adult use, with shorter sizes available for pediatric or smaller patients. It is a transparent or clear hub to allow visualization of fluid or air, ensuring proper positioning. Epidural Needle is commonly used for administering epidural anesthesia or for placing an epidural catheter.
-
Material Quality
It is manufactured from high-quality stainless steel to prevent bending or breaking during insertion.
-
Needle Bore
It is wide enough to pass a catheter smoothly without damaging it. While ensuring the stability of the catheter during and after insertion.
-
Epidural Catheter Compatibility
It is designed to work with flexible catheters to give medication either continuously or at regular intervals with breaks in between.
-
Highly Suitable for Epidural Anesthesia
It is Ideal for delivering anesthetics during childbirth, lower body surgeries, or pain management procedures.
-
Anesthetic Opioid Synergy
It refers to the combined use of anesthetics (drugs that block sensation) and opioids (pain-relieving medications) to achieve enhanced pain relief.
Uses of an Epidural Needle :
- Labor Pain Relief: It provides epidural anesthesia during the process of childbirth, including vaginal and cesarean deliveries.
- Surgical Anesthesia: It is used for lower body procedures as an alternative to general anesthesia.
- Chronic Pain Management: It is used to deliver medication for conditions like back pain and sciatica.
- Post-Surgical Pain Relief: It is used to inserts a catheter in the epidural space for continuous pain management after surgeries.
- Regional Anesthesia: It is used for bloking the pain in specific areas while keeping the patient awake.
EPIDURAL NEEDLE Versus SPINAL NEEDLE
| Aspect | Epidural Needle | Spinal Needle |
| Purpose | It is used to deliver medication into the epidural space outside the dura mater. | It is used to inject medication directly into the cerebrospinal fluid (CSF) in the subarachnoid space. |
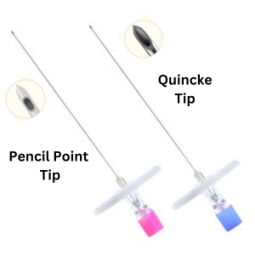
| Tip Design | It is blunt, non-cutting tip (e.g., Tuohy needle) to prevent dura puncture and allow epidural catheter placement. | It is fine, sharp or pencil-point tip (e.g., Quincke, Whitacre) designed to pierce the dura for precise CSF access. |
| Medication Delivery | Medication spreads in the epidural space for gradual, broader pain relief. | Medication directly enters the CSF, providing rapid onset and a more defined sensory block. |